Medicare Advantage (MA) is the private plan option in the Medicare program. Enrollment in the program has grown nearly 10% a year in recent years and now tops 25 million. More than one-third of Medicare beneficiaries (people with Medicare) have opted into MA, and the total number of MA enrollees is expected to top 30 million in the next few years.
While MA plans have long offered enrollees supplemental benefits — such as vision, hearing and limited dental coverage — recent regulatory actions enable MA plans to offer a wider array of benefits. These include permitting plans to make the benefits disease- or condition-specific. The Centers for Medicare and Medicaid Services (CMS) also expanded the range of permissible benefits to include Special Supplemental Benefits for Chronic Illness (SSBCI). SSBCIs are non-healthcare related benefits for plan members for chronic and disabling diseases. SSBCIs include air conditioning for people with severe asthma and healthy foods for plan members with diabetes.
As with all major healthcare policy changes, it takes a while for the market to embrace the full potential of the newly enabled innovations. Such is the case with disease- and condition-specific benefits; less than 10% of plans offered the new SSBCI benefits in 2020.
Last fall, when the 2021 MA benefits data first became available, we reported on important changes in supplemental benefit usage in MA plans. Now that CMS has released the condition-specific and SSBCI benefits, this report completes our analysis of the 2021 MA supplemental benefit landscape.
Condition-Specific Benefits
The total number of condition-specific “flex” benefits rose from 1850 in 2020 to 2180 in 2021. Similar to 2020, the most common conditions served by specialized benefits include diabetes, congestive health failure (CHF), dementia and chronic obstructive pulmonary disease (COPD), four relatively prevalent and expensive conditions. Beyond these conditions, there are some noticeable changes between 2021 and 2020. Likely because of the COVID-19 Public Health Emergency, 230 MA plans are offering benefits related to anxiety, depression and substance use disorders in 2021 (there were no such condition-specific benefits in 2020). There were also significant increases in the number of plans offering condition-specific benefits for cancer, hyperlipidemia, liver disease and a history of falls.
In Table 1 below, we list the top ten most prevalent diseases and their percent change from 2020 into 2021.
| Figure 1: Most Prevalent Diseases |
|||
| DISEASES |
2021 TOTAL |
2020 TOTAL |
PERCENT GROWTH |
|---|---|---|---|
| Diabetes |
517 |
473 |
9% |
| Congestive Heart Failure (CHF) |
266 |
256 |
4% |
| Anxiety, Depression, or Substance Abuse Disorder |
230 |
0 |
|
| Chronic Obstructive Pulmonary Disease (COPD) |
168 |
198 |
-15% |
| Hypertension |
99 |
88 |
13% |
| Opiate Use Disorder |
84 |
88 |
-5% |
| Coronary Artery Disease |
70 | 97 |
-28% |
| Pre-diabetes |
62 |
60 |
3% |
| Cellulitis | 48 |
48 |
0% |
| Pneumonia |
48 |
48 |
0% |
Plans may either choose to offer condition-specific benefits in either the form of reduced cost-sharing or additional supplemental benefits. Furthermore, reduced cost-sharing benefits can be for either Medicare-covered benefits or non-Medicare supplemental benefits. We found that MA plans are more likely to reduce cost-sharing for Medicare-covered benefits. In total, MA plans are offering 97 different types of condition-specific benefits. No single benefit type comprises greater than 10% of the total — showing an immature market still undergoing considerable experimentation.
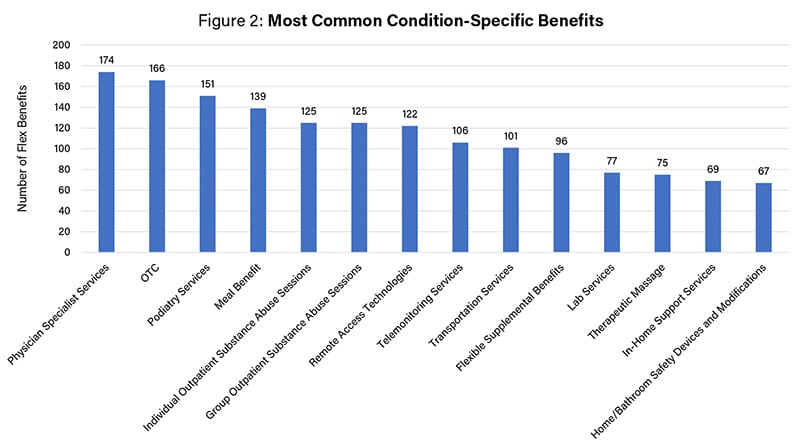
The benefits offered for members with these particular conditions ranged considerably from reduced cost-sharing on covered services (e.g., physician services, podiatry, lab services) to expansions of widely available supplemental benefits (e.g., OTC, transportation, meals) to newer benefits offered for chronic and disabling conditions (such as in-home support). In Figure 2 below, we list the most common condition-specific benefits in 2021.
Condition-Specific Benefits with Prerequisites
MA plans are permitted to establish prerequisites that must be met in order to access the condition-specific benefit. Care management programs, for example, are helpful in successfully controlling certain chronic diseases. For this reason, a MA plan might want to link access to a condition-specific benefit to participation in the care management program. Interestingly, 28 plans require both a plan-designated high-value provider and participation in a care management program as a prerequisite. In Figure 3 below, we show that the majority of plans do not tie condition-specific benefits to a prerequisite.
| Figure 3 |
|
| PREREQUISITE | TOTAL NUMBER OF PLANS |
|---|---|
| None | 1101 |
| High Value Provider | 34 |
| Participation in a Care Management Program |
891 |
| Other | 4 |
SSBCIs
As discussed above, MA plans can provide non-health related benefits when they are focused on a chronic and disabling condition. The initial uptake of these benefits in 2020 was modest; only 245 plans offered an SSBCI. In contrast, in 2021, SSBCIs are offered in 831 plans (out of approximately 5,200 total plans). In Figure 4 below, we show the most common SSBCIs in 2020.
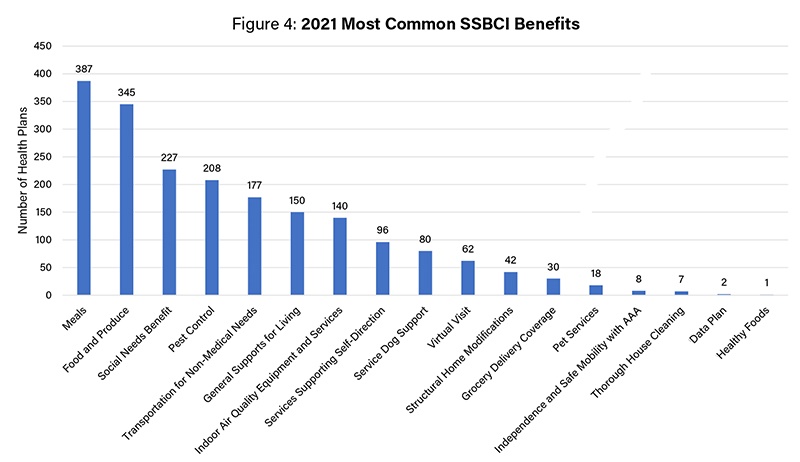
The SSBCIs that are being used far more often in 2021 include: meals, food and produce, social need benefits and air conditioning. SSBCIs that are newly approved in 2021 include: data plans, pet services, housing cleanings and virtual companion visits. This illustrates the rapid acceptance of benefits that are tied to addressing social determinants of health. It is important to note that a majority of health plans offering these benefits combine them with other benefits and services; social determinant-focused SSBCIs are best considered within a broader strategy for serving vulnerable members.
Rate of Adoption Across MA Organizations
We also explored the frequency of adoption of condition-specific benefits across Medicare Advantage organizations and discovered great variation. Among the seven Medicare Advantage parent organizations offering plans in many states, condition- and disease-specific benefits are offered in 724 out of 3829 plans. Each of these seven parent organizations offer condition- and disease-specific benefits in at least 27 plans. In contrast, many local and regional MA organizations are not yet utilizing condition-specific benefits at all — though a few are embracing benefit innovations at a higher proportional rate than the national plans.
Other promising benefit flexibilities — such as using benefits to drive members to "high value" providers or offering benefits based on low-income status — are only in the earliest state of adoption by MA organizations. Benefits contingent on low-income status, for example, are available to less than 13,000 low-income MA plan members (this is partly because low-income contingent benefits are only available to MA plans participating in CMS’s VBID model).
Beyond benefits, MA plans are also increasingly offering innovations through other vehicles — care management programs, reward and incentive programs, and value-added services. New flexibilities around drug formularies, provider marketing and provider network adequacy are other frontiers where adoption of new flexibilities is uneven. We have long discussed the "arms race" nature of innovation adoption in the competitive MA market. If an innovations arms race is underway, not all plans are comparably armed in 2021.
If Medicare Advantage innovations interest you as much as us, or if you would like to learn more about our MA benefits database and bibliography of benefit innovations (nearing 1,000 articles and announcements), contact the authors.
.svg?rev=a492cc1069df46bdab38f8cb66573f1c&hash=2617C9FE8A7B0BD1C43269B5D5ED9AE2)

